Effect of Race Upon Organ Donation and Recipient Survival in Liver Transplantation, Nov 1990:
Abstract
The effect of the race of the donor on organ donation and on the outcome of clinical liver transplantation has not been addressed previously. The aims of this study were to determine: (1) the number of organs donated by each of the major racial groups of the United States, (2) the outcome of transplantation of these organs across racial groups, and (3) the pattern of liver disease that required transplantation in each of these racial groups. A significantly higher proportion of organs were donated by white non-Hispanic Americans than either black or Hispanic Americans. There was no significant difference in survival when an organ was transplanted between black and white Americans and vice versa.
Currently, donors for liver transplantation are matched with recipients only according to ABO blood group compatibility and body size. Nonetheless, it is well known that man as a biological species is polymorphic, with significant variation occurring within the species. Despite genetic differences in the prevalence of blood groups and HLA antigens between the various races, the effect of the race of the donor and the race of the recipient on the outcome of clinical OLTx has never been investigated.
A retrospective analysis of all adult patients undergoing their first OLTx at the Presbyterian University Hospital of the University of Pittsburgh between January 1, 1981, and December 31, 1988
The race of the donor was determined by what the family members considered was their racial grouping, while that of the recipient was determined by what the patients considered their racial group to be. For the purpose of this study, a transplant failure was defined as a graft failure leading to retransplantation and/or the patients death within 60 days of the initial liver transplant.
The total number of livers donated by blacks (69) was far less than that by whites 795 (Hispanic and non-Hispanic). Of the 51 black recipients, only 5 (10%) received an organ donated by a black, while 46 (90%) received an organ donated by a white; conversely of the 813 white recipients, 749 (92%) received an organ from a white donor while 64 (8%) received an organ from a black donor (P < 0.001). The total number of organs donated by blacks for either black or white recipients was far less than that observed for whites and is well below their population fraction.
A breakdown of the white population into Hispanic and non-Hispanic groups (Table 3) shows that the number of organs donated by the Hispanic group is even smaller than that donated by the black population. Thus, most donors are white non-Hispanics and both Hispanic and black recipients are most likely to receive an organ donated by a white who is non-Hispanic.
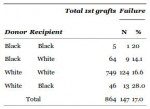
PubMed Central, Table 1: Dig Dis Sci. 1990 November; 35(11): 1391–1396.
This table indicates the failure rate of black recipients of White livers is twice the rate for Whites recipients of any liver.
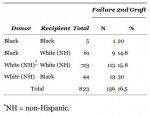
PubMed Central, Table 2: Dig Dis Sci. 1990 November; 35(11): 1391–1396.
This table excludes “hispanics”. A more honest term would be mestizo, meaning “people with a various degrees of Caucasian, Amerindian and African admixture”. The black recipient failure rate is still roughly twice the White failure rate. The article says:
The failure rate for an organ transplanted from a black donor into a white recipient was 14.1% (14.8% in the case of a white non-Hispanic) while the failure rate for an organ obtained from a white donor and transplanted into a black was 28% (30% for white non-Hispanics). These differences were not significant.
PubMed Central, Table 3: Dig Dis Sci. 1990 November; 35(11): 1391–1396.
This table directly contrasts White with “hispanic”. Note that it indicates the White failure rate is more than doubled when the donor is “hispanic”.
PubMed Central, Table 5: Dig Dis Sci. 1990 November; 35(11): 1391–1396.
This table indicates that the mixed race cases consistently result in higher failure rates.
Because of the small numbers involved, there was no statistically significant difference in the failure rate for recipients with either PBC, PSC, or AHF among the various races. Among recipients transplanted for PNC, no differences in the failure rate was evident when the donor and recipient pairs were either matched or mismatched for race.
When race was considered in addition to other variables such as age, sex, and ABO blood groups, no difference in outcome was found, although the number of blacks within each of these subsets was small.
DISCUSSION
No data exist with respect to the outcome of organ donation between racial groups in clinical liver transplantation. This is related in part to the difficulty in classifying individuals in one or another racial group based solely upon their physical characteristics—commonly referred to as the “typological approach.” Our definition was determined by what the patient or the donor’s family members considered themselves to be.
The main difficulty with the “typological approach”, or for that matter most any empirical approach to race, is that it runs afoul the anti-“racist” dogma that race doesn’t exist or doesn’t matter or is a social construct of oppressive Whites. Race is not supposed to be real or important or objective despite all the indications that it is. The fact that any deliberate measure of the actual effects of such obvious biological differences could be put off for so long, despite the potential (and apparently substantial) life-threatening impact, is a good indication how all-important anti-“racist” ideology has become.
The present study confirms the low rate of donation of livers among blacks and Hispanics. It also shows that transplantation across racial groups has no effect upon the transplant outcome. The importance of determining the severity of the recipient’s illness and correcting for such is also illustrated in this study. The apparent higher failure rate for organs obtained from white donors and transplanted into black recipients was due entirely to the fact that a higher proportion of the black recipients who died were more seriously ill (4–6 on UNOS scale) than were the white recipients who were transplanted in this series (Table 4). However, a difference in survival rate for transplants performed between white Hispanics and white non-Hispanics also was noted. The numbers within this group are small, however, and thus no definitive conclusion can be drawn from the data.
The genetic differences owing to race per se are not considered to be major, as the genetic variability within each race is greater than the variability between the races. Moreover, it has been variously estimated that black Americans have a 30–50% chance of having a white ancestor (10). Because of this fact and because of the findings in this study, the likelihood of graft failure solely as a result of the presence of a genetic difference between the race of the donor and recipient is not tenable. This conclusion is consistent with studies recently reported for renal transplantation from our center (11). Thus transplantation of organs across racial groups can be performed without fear of an additional problem occurring as a result of some inherent difference between the donor and recipient races. Our data indicate that the major problem in success of liver transplantation is the severity of the illness of the recipient immediately prior to the transplant.
The numbers in the tables contradict the textual denials which accompany them. The reasons provided – statistical insignificance, severity of illness – are not accompanied by any detailed exposition. The raw numbers indicate a consistently higher failure rate for cross-race transplants, and at the very least suggest that more deliberate research is warranted.
They claim similar results for kidney transplants. Similarly flawed perhaps. The problem with cross-race kidney transplants is described in the following reports.
Donor Race May Impact Kidney Transplant Survival, Oct 2009:
“We found that transplant between races had better outcomes than transplant across races,” says Anita Patel, M.D., transplant nephrologist at Henry Ford Hospital Transplant Institute and lead author of the study.
By regression analysis, the non-black recipients who received a kidney from black donors had a significant lower survival rate compared to those who received a kidney from a non-black donor (hazard ratio 1.111, p=0.014) after adjusting for all known variables.
“Hepatitis C infection in the donor or recipient was seen as a significant risk factor for mortality,” says Dr. Patel.
Dr. Patel presented a similar study earlier this year which looked at race and the effect on renal allograft survival in different donor/recipients pairs. In that study, Dr. Patel found an increased risk in graft failure in non-black recipients of non-heart beating black donor kidneys. They appeared to have a two-fold increased risk of graft failure.
Twelve percent of living donors are African-American.
“It’s been long observed that kidneys taken from some black donors just don’t last as long as those taken from non-black donors, and the reason for that has not been known,” said Barry I. Freedman, M.D., John H. Felts III Professor and senior investigator. “This study reveals that the genetic profile of the donor has a marked affect on graft survival after transplantation. We now know that these organs aren’t failing because they came from black donors, but rather because they came from individuals with two copies of a specific recessive gene.”
Long observed, and long ignored.
The researchers identified that kidneys from donors who had specific coding changes in a gene called apolipoprotein L1 (APOL1) did not last as long after transplant as those from donors without these changes. These coding changes in the APOL1 gene that affect kidney transplant function are found in about 10 to 12 percent of black individuals. Recent studies, led by Freedman and his colleagues, have shown that these genetic changes are associated with an increased risk of kidney disease, which prompted researchers to investigate the role of these changes in transplant success.
“In looking at the records and follow-up of the recipients of these organs, we accounted for all the usual factors that are known to contribute to more rapid loss of kidney function after transplant,” said Freedman, chief of the section on nephrology. “What we found was that the kidney disease-causing risk variants in APOL1 were the strongest predictor of graft loss after transplant. The effect of having two copies of this gene was stronger than the impact of genetic matching between donor and recipient, the amount of time the organ was out of the body, and the antibody levels. APOL1 dwarfed all these other factors known to affect survival.”
A more honest title for this article would be, “Race denial causes death”, or “Genetic factors finally discovered despite race denial”.
There is no “black gene”. There are many black genes. This is one of them.
The problem is avoided entirely by avoiding cross-race transplants.
Institute of Human Values in Health Care • Medical University of South Carolina
The issue of race poses special problems in transplantation. Because of the prevalence of hypertensive renal disease in the black population, that group has a disproportionately high representation on the kidney transplant waiting list. While blacks compose 12% of the general population, they comprise 37% of the kidney transplantation waiting list, yet receive 25% of the kidney transplants. Other organs are not so disproportionate.
A variety of factors contribute to differences among races: biological, medical, social, and personal. Biological factors include different rates of ABO blood groups within races, as well as differences in major histocompatibility complex antigens. Because of these differences, organs from black donors have a better match with potential black recipients than white. Blacks have a lower donation rate than whites, for reasons discussed in more detail below, contributing to fewer available biologically compatible organs for blacks than for whites.
Confirms racial differences reflected in disparate incidence of disease, distribution of blood types, donation rates.
Such a program is likely to disproportionately benefit the rate of transplantation in the black community. Blacks donate organs at a lower rate than whites. There are many reasons for this, but prominent among them are distrust within the black community of the health care system and of medical authority, and the belief that donated organs from blacks will go to other races. A system in which black persons could specify that their organs could go only to other blacks would give them a special reason to donate. An additional benefit of an increase in black donation rate is that blood groups and histocompatibility antigens have different distributions in different races. Therefore, as the black donation rate goes up, the number of transplants into blacks will increase, and longevity of the implanted organs will improve as well.
As with blood, an examination of organ transplants indicates that race not only exists but has significant consequences. When something is perceived to be somehow negative for non-Whites the “medical community” argues openly and unabashedly to help them, even if that means acknowleding race and racial differences. Meanwhile, concern for White lives is pathologized and demonized. This dishonest regime is called anti-“racism”. Anti-“racism” causes White deaths.
The podcast will be broadcast and available for download on Tuesday at 9PM ET.
Podcast: Play in new window | Download











There are so many layers of PC propaganda on top of the information we need that it is almost opaque. I have a deep suspicion that the stats selected for these studies weren’t random or unbiased.
White altruism is a wonderful characteristic in an all White Society. It is deadly in a mixed race society.
The part about blacks not donating because of a chance that it would go to another race. I don’t believe it! Maybe in a few instances.
I’ve talked and listened to blacks talk about organ donation. They have a superstitious belief that they won’t be ‘whole’ if they are buried without all their organs. That their spirit will be mixed with that of another person’s. Some kind of Voodoo like belief.
There’s a lot of superstition in the black community. Most of them work to conceal it, but it is still there.
Race is the third rail in Western Science. Anyone in the scientific community who touches the subject can expect to be defunded, ostracized and a stake driven through any chance of professional advancement.